Well, its been a while since I've posted on here. Just an update ...
I didn't need a treatment last month which was wonderful! I haven't had a leak in my right eye since January. We've just been treating for safety's sake the past several months. Dr. Gindzen says my right eye look great. God has truly answered so many prayers! (My left eye is actively leaking but since I have a permanent scar from the laser treatments, we aren't going to be treating the leak).
The VISION 2008 seminary was wonderful! Steve and I had a great time and learned so much about retinal diseases. We met some great people and their stories were so encouraging. I really has a new outlook on my condition after the conference.
Another recent development is that I'm 7 weeks pregnant. I have to tell my RS tomorrow and I know he'll be disappointed. We were supposed to wait a couple of years for a better treatment ... one which could be administered while pregnant. Well, sometimes God has different plans and this was one of them. I'm praying that God will take care of my eyes and give us a healthy baby. I know if there is one cure out there for me, its God. I have full faith that He will prevail over this disease.
Please keep us in your prayers as we go through the next 33 weeks.
~ Always in Christ, Rebecca
Thursday, September 18, 2008
Subscribe to:
Comments (Atom)
Another victim to POHS
My name is Rebecca. I was officially diagnosed with Ocular Histoplasmosis Syndrome in January of 2008. I grew up in Nashville, Tennessee and had never heard of the fungus Histoplasma Capsulatum until after moving to Grand Rapids, Michigan in August of 2007.
It is my hope from this blog that I can provide information to others about this terrible disease and urge people within the "Histo Belt" to check their sight on a regular basis.
It is my hope from this blog that I can provide information to others about this terrible disease and urge people within the "Histo Belt" to check their sight on a regular basis.
INTERESTING VIDEOS
I've added some interesting videos of different retinal surgeries. I will warn you that these can be graphic, but if you're interested in knowing what surgeries have been done and how they work, take a peek!
Vitrectomy for Vitreous Opacities (Floaters)
Floaters - What are they? How do they happen?
Removal of Subretinal Neovascular Membrane due to OHS
Vitrectomy Surgery
Vitrectomy Surgery allows the Retina Surgeon to work inside of the eye and repair damage caused by a variety of diseases. The vitreous is the jelly inside the eye and is removed during the vitrectomy. YOU DO NOT NEED YOUR VITREOUS. The vitreous is important when the eye forms as a fetus grows into a baby, but it does nothing good for you after that. The vitreous is replaced with a salt solution or gas or oil and your body replaces the salt solution or gas in the vitreous cavity over a week or two.
Some vitrectomies can be performed using very small 25 gauge instruments. Most are done with 20 gauge instrument. Once the vitreous is removed, instruments like picks, forceps, lasers, and cautery can be used inside the eye to help fix problems like macular pucker, macular hole, retinal detachment, vitreous hemorrhage, diabetic retinal disease, infection, retained lens fragments and so on.
Vitrectomy surgery in our practice is usually done with local anesthesia and sedation. Since you will be sedated, YOU CANNOT EAT the morning of surgery. You will be sedated and your eye will be anesthetized. You will be monitored by an anesthesiologist or nurse anesthetist. After surgery you will have to wear a patch and shield over the eye until your appointment the following day.
If you have a retinal detachment and your doctor puts a gas or oil to hold your retina in place, you will have to hold your head in a certain position and also look in a certain position for the surgery to work. This is also true of surgery for macular holes which requires face down positioning.
After your patch is removed during your post-operative visit, you will need to take eye drops. If during the week after surgery, your eye starts to hurt more or vision starts to decline, you should call our office since that can indicate a problem with infection or elevated intraocular pressure. If you see a new shadow after surgery you need to call so we can check to make sure you do not have a retinal detachment.
Using modern microsurgical techniques, your retinal surgeon is able to repair many macular and retinal problems that were once thought unfixable. Your physician can tell you what the success rates are for your surgery including the possibility of some vision improvement and the possibility of a lot of vision improvement.
After any eye surgery there is a risk of infection, bleeding, and retinal detachment. Also, the intraocular pressure in the eye can sometimes rise necessitating extra post-operative eye drops. Make sure to call our office if you are having any problems.
Some vitrectomies can be performed using very small 25 gauge instruments. Most are done with 20 gauge instrument. Once the vitreous is removed, instruments like picks, forceps, lasers, and cautery can be used inside the eye to help fix problems like macular pucker, macular hole, retinal detachment, vitreous hemorrhage, diabetic retinal disease, infection, retained lens fragments and so on.
Vitrectomy surgery in our practice is usually done with local anesthesia and sedation. Since you will be sedated, YOU CANNOT EAT the morning of surgery. You will be sedated and your eye will be anesthetized. You will be monitored by an anesthesiologist or nurse anesthetist. After surgery you will have to wear a patch and shield over the eye until your appointment the following day.
If you have a retinal detachment and your doctor puts a gas or oil to hold your retina in place, you will have to hold your head in a certain position and also look in a certain position for the surgery to work. This is also true of surgery for macular holes which requires face down positioning.
After your patch is removed during your post-operative visit, you will need to take eye drops. If during the week after surgery, your eye starts to hurt more or vision starts to decline, you should call our office since that can indicate a problem with infection or elevated intraocular pressure. If you see a new shadow after surgery you need to call so we can check to make sure you do not have a retinal detachment.
Using modern microsurgical techniques, your retinal surgeon is able to repair many macular and retinal problems that were once thought unfixable. Your physician can tell you what the success rates are for your surgery including the possibility of some vision improvement and the possibility of a lot of vision improvement.
After any eye surgery there is a risk of infection, bleeding, and retinal detachment. Also, the intraocular pressure in the eye can sometimes rise necessitating extra post-operative eye drops. Make sure to call our office if you are having any problems.
What is Histoplasmosis?
Histoplasmosis is a disease caused when airborne spores of the fungus Histoplasma capsulatum are inhaled into the lungs, the primary infection site. This microscopic fungus, which is found throughout the world in river valleys and soil where bird or bat droppings accumulate, is released into the air when soil is disturbed by plowing fields, sweeping chicken coops, or digging holes.
Histoplasmosis is often so mild that it produces no apparent symptoms. Any symptoms that might occur are often similar to those from a common cold. In fact, if you had histoplasmosis symptoms, you might dismiss them as those from a cold or flu, since the body's immune system normally overcomes the infection in a few days without treatment.
However, histoplasmosis, even mild cases, can later cause a serious eye disease called ocular histoplasmosis syndrome (OHS), a leading cause of vision loss in Americans ages 20 to 40.
Histoplasmosis is often so mild that it produces no apparent symptoms. Any symptoms that might occur are often similar to those from a common cold. In fact, if you had histoplasmosis symptoms, you might dismiss them as those from a cold or flu, since the body's immune system normally overcomes the infection in a few days without treatment.
However, histoplasmosis, even mild cases, can later cause a serious eye disease called ocular histoplasmosis syndrome (OHS), a leading cause of vision loss in Americans ages 20 to 40.
Where does Ocular Histoplasmosis Syndrome come from?
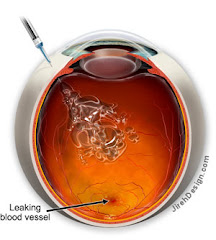
Scientists believe that Histoplasma capsulatum (histo) spores spread from the lungs to the eye, lodging in the choroid, a layer of blood vessels that provides blood and nutrients to the retina. The retina is the light-sensitive layer of tissue that lines the back of the eye. Scientists have not yet been able to detect any trace of the histo fungus in the eyes of patients with ocular histoplasmosis syndrome. Nevertheless, there is good reason to suspect the histo organism as the cause of OHS.
What are the symptoms of OHS?
OHS usually has no symptoms in its early stages; the initial OHS infection usually subsides without the need for treatment. This is true for other histo infections; in fact, often the only evidence that the inflammation ever occurred are tiny scars called "histo spots," which remain at the infection sites. Histo spots do not generally affect vision, but for reasons that are still not well understood, they can result in complications years--sometimes even decades--after the original eye infection. Histo spots have been associated with the growth of the abnormal blood vessels underneath the retina.
In later stages, OHS symptoms may appear if the abnormal blood vessels cause changes in vision. For example, straight lines may appear crooked or wavy, or a blind spot may appear in the field of vision. Because these symptoms indicate that OHS has already progressed enough to affect vision, anyone who has been exposed to histoplasmosis and perceives even slight changes in vision should consult an eye care professional.
In later stages, OHS symptoms may appear if the abnormal blood vessels cause changes in vision. For example, straight lines may appear crooked or wavy, or a blind spot may appear in the field of vision. Because these symptoms indicate that OHS has already progressed enough to affect vision, anyone who has been exposed to histoplasmosis and perceives even slight changes in vision should consult an eye care professional.
How is OHS Diagnosed?
An eye care professional will usually diagnose OHS if a careful eye examination reveals two conditions: (1) The presence of histo spots, which indicate previous exposure to the histo fungus spores; and (2) Swelling of the retina, which signals the growth of new, abnormal blood vessels. To confirm the diagnosis, a dilated eye examination must be performed. This means that the pupils are enlarged temporarily with special drops, allowing the eye care professional to better examine the retina.
If fluid, blood, or abnormal blood vessels are present, an eye care professional may want to perform a diagnostic procedure called fluorescein angiography. In this procedure, a dye, injected into the patient's arm, travels to the blood vessels of the retina. The dye allows a better view of the CNV lesion, and photographs can document the location and extent to which it has spread. Particular attention is paid to how close the abnormal blood vessels are to the fovea.
If fluid, blood, or abnormal blood vessels are present, an eye care professional may want to perform a diagnostic procedure called fluorescein angiography. In this procedure, a dye, injected into the patient's arm, travels to the blood vessels of the retina. The dye allows a better view of the CNV lesion, and photographs can document the location and extent to which it has spread. Particular attention is paid to how close the abnormal blood vessels are to the fovea.
Information on systemic histoplasmosis can be obtained from:
The National Institute of Allergy and Infectious Diseases (NIAID)The National Institutes of Health
Building 31, Room 7A50
31 Center Drive, MSC 2520
Bethesda, MD, 20892-2520
Telephone: 301-496-5717
Website: http://www.niaid.nih.gov
Building 31, Room 7A50
31 Center Drive, MSC 2520
Bethesda, MD, 20892-2520
Telephone: 301-496-5717
Website: http://www.niaid.nih.gov