Well, its been a while since I've posted on here. Just an update ...
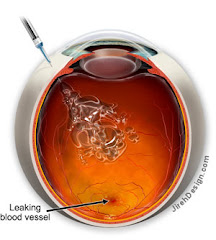
I didn't need a treatment last month which was wonderful! I haven't had a leak in my right eye since January. We've just been treating for safety's sake the past several months. Dr. Gindzen says my right eye look great. God has truly answered so many prayers! (My left eye is actively leaking but since I have a permanent scar from the laser treatments, we aren't going to be treating the leak).
The VISION 2008 seminary was wonderful! Steve and I had a great time and learned so much about retinal diseases. We met some great people and their stories were so encouraging. I really has a new outlook on my condition after the conference.
Another recent development is that I'm 7 weeks pregnant. I have to tell my RS tomorrow and I know he'll be disappointed. We were supposed to wait a couple of years for a better treatment ... one which could be administered while pregnant. Well, sometimes God has different plans and this was one of them. I'm praying that God will take care of my eyes and give us a healthy baby. I know if there is one cure out there for me, its God. I have full faith that He will prevail over this disease.
Please keep us in your prayers as we go through the next 33 weeks.
~ Always in Christ, Rebecca
Thursday, September 18, 2008
Wednesday, July 2, 2008
VISIONS 2008 Convention in Washington, DC
On August 8-10, Steve and I have the opportunity to go to the Vision 2008 Retinal Disease Convention in DC. What a blessing from God! Below is the link to the website if you'd like to attend or learn more about it.
http://www.blindness.org/VISIONS/
Some of the Doctors Speaking at VISIONS 2008 Include:
David Gamm, M.D., Ph.D., University of Wisconsin Hospitals and Clinics
William Kimberling, Ph.D., National Usher Syndrome Center
Janet Sunness, M.D., Greater Baltimore Medical Center
David Birch, Ph.D., Retina Foundation of the Southwest
Jacque Duncan, M.D., UCSF School of Medicine
J. Jill Hopkins, M.D., Retina-Vitreous Associates
Byron Lam, M.D., Bascom Palmer Eye Institute
Shalesh Kaushal, M.D., Ph.D., University of Florida
Dennis R. Hoff man, Ph.D., Retina Foundation of the Southwest
Linda Lemieux, Advanced Cell Technology
Estelle Condra, Author and Motivational Speaker
Rafael Caruso, M.D., National Eye Institute
Emily Chew, M.D., National Eye Institute
Morton Goldberg, M.D., National Neurovision Research Institute
Mary Elizabeth Hartnett, M.D., UNC School of Medicine
Meira Meltzer, M.A., M.S., National Eye Institute
http://www.blindness.org/VISIONS/
Some of the Doctors Speaking at VISIONS 2008 Include:
David Gamm, M.D., Ph.D., University of Wisconsin Hospitals and Clinics
William Kimberling, Ph.D., National Usher Syndrome Center
Janet Sunness, M.D., Greater Baltimore Medical Center
David Birch, Ph.D., Retina Foundation of the Southwest
Jacque Duncan, M.D., UCSF School of Medicine
J. Jill Hopkins, M.D., Retina-Vitreous Associates
Byron Lam, M.D., Bascom Palmer Eye Institute
Shalesh Kaushal, M.D., Ph.D., University of Florida
Dennis R. Hoff man, Ph.D., Retina Foundation of the Southwest
Linda Lemieux, Advanced Cell Technology
Estelle Condra, Author and Motivational Speaker
Rafael Caruso, M.D., National Eye Institute
Emily Chew, M.D., National Eye Institute
Morton Goldberg, M.D., National Neurovision Research Institute
Mary Elizabeth Hartnett, M.D., UNC School of Medicine
Meira Meltzer, M.A., M.S., National Eye Institute
Tuesday, June 17, 2008
Appointment - June 13, 2008
My appointment on June 13th went very well. My last treatment was on May 1st, so I have officially gone 6 weeks without a treatment. Dr. Gindzen said my right eye looked great and that the Avastin injections worked perfectly. Now, we are monitoring the eye at 4 week intervals to make sure there is no activity nor new bleeds.
The only trouble I am having is with the vitreous. The jelly-like substance has become weakened (as I explained in my previous blog) causing floaters. The floaters are causing the vision to be very distorted making it difficult to drive and read, especially at night or when my eye is tired. I have three options when it comes to the vitreous distortion.
1) Learn to live with it as I did when I lost my central vision in my left eye.
2) Continue having the Avastin shots every 4 weeks allowing the vitreous to continue to weaken so gravity will eventually pull it down, and it won't be floating the way it is now. This process of weakening could take several years and during that time, my vision would get increasingly worse. Currently the weakened vitreous has pulled away from the back of my eye but is still too firm for gravity, so it is just floating there distorting the vision instead of being pulled to the bottom of my eye by gravity.
3) Vitrectomy surgery. I have put information about this surgery at the bottom of the blog along with a video of this surgery being done on an OHS patient while removing a subretinal scar. This surgery comes with its risks ... the worse being complete blindness in that eye from an infection (1 out of 100,000). With not having my left eye to fall back on, this is an even higher risk for me.
At this point, I have chosen to live with the distortion. It took me a while to get used to losing the vision in my left eye, but I got used to it with the help of 20/20 in my right. Fortunately, the vitreous is only affecting the peripheral vision in my right eye, so I can still see 20/20. I'm not willing to risk that until the vitreous gets worse and/or impairs my macula.
The surgery is interesting though, and if you'd like to see it, watch the video at the bottom. If blood makes you queezy, I'd suggest just reading about it.
The only trouble I am having is with the vitreous. The jelly-like substance has become weakened (as I explained in my previous blog) causing floaters. The floaters are causing the vision to be very distorted making it difficult to drive and read, especially at night or when my eye is tired. I have three options when it comes to the vitreous distortion.
1) Learn to live with it as I did when I lost my central vision in my left eye.
2) Continue having the Avastin shots every 4 weeks allowing the vitreous to continue to weaken so gravity will eventually pull it down, and it won't be floating the way it is now. This process of weakening could take several years and during that time, my vision would get increasingly worse. Currently the weakened vitreous has pulled away from the back of my eye but is still too firm for gravity, so it is just floating there distorting the vision instead of being pulled to the bottom of my eye by gravity.
3) Vitrectomy surgery. I have put information about this surgery at the bottom of the blog along with a video of this surgery being done on an OHS patient while removing a subretinal scar. This surgery comes with its risks ... the worse being complete blindness in that eye from an infection (1 out of 100,000). With not having my left eye to fall back on, this is an even higher risk for me.
At this point, I have chosen to live with the distortion. It took me a while to get used to losing the vision in my left eye, but I got used to it with the help of 20/20 in my right. Fortunately, the vitreous is only affecting the peripheral vision in my right eye, so I can still see 20/20. I'm not willing to risk that until the vitreous gets worse and/or impairs my macula.
The surgery is interesting though, and if you'd like to see it, watch the video at the bottom. If blood makes you queezy, I'd suggest just reading about it.
Wednesday, June 4, 2008
June Update
Well, as of today, I've officially gone six days without a treatment since March. I guess this is a great thing b/c I don't think I've had a new bleed since not getting an injection on May 29th. I've had three treatments so far at exactly 4 week intervals and my next appointment is June 13th. So, we are trying to see where the growths are at 6 weeks instead of "pre-treating" at 4.
I'm stuck between a rock and a hard place with these treatments. The Avastin is working as far as keeping the growths away, but the side effects of the injections are causing just as much trouble as the bleed would. From what I understand, the injections are weakening the vitreous causing the jelly-like fluid to break away from the back of the eye and float into my vision line. These floaters are causing my peripheral vision to be very distorted and blurry ... the only difference being these floaters float (or jiggle) around whereas a bleed stays in one spot.
Floaters are normal in an elderly person b/c as you age, the vitreous naturally weakens. But in a 26 year old, that part of your eye is very firm. The vitreous fluid is like jelly and when it pulls away from the back of the eye, it can cause retinal tears. These tears can then lead to retinal detachment. So in essense, these injections are turning my eyes into that of a 75 year old and as far as I'm concerned, doing a much harm as good.
I'm working with my PCP & RS on getting to a doctor at the Cleveland Clinic.. We have to submit several letters of recommendation to my insurance company in order to convince them to cover the treatments out-of-network. I'm also hoping that Dr. Gindzen can convince the insurance company to cover Lucentis injections since that's the FDA drug instead of Avastin, which is what I'm currently using. Hopefully the smaller molecules will do less damage and will lessen the floaters.
Due to the floaters and vision loss from my first bleed, I'm starting to have alot of trouble driving, esp at night or when my eyes are tired. I've been invited to a luncheon by the Disability Advocates this month, so hopefully I can start getting involved with that group and advocate for better public transportation in our area of town. Its a great group in Grand Rapids, and they do alot of good work for the disable.
So, that's about it. I would love some feedback from others struggling with POHS, especially if you are dealing with floaters that won't go away. Otherwise, thank you for all your prayers and please don't stop praying for my struggle with this disease as well as others who deal with this every day.
God Bless!
Rebecca
I'm stuck between a rock and a hard place with these treatments. The Avastin is working as far as keeping the growths away, but the side effects of the injections are causing just as much trouble as the bleed would. From what I understand, the injections are weakening the vitreous causing the jelly-like fluid to break away from the back of the eye and float into my vision line. These floaters are causing my peripheral vision to be very distorted and blurry ... the only difference being these floaters float (or jiggle) around whereas a bleed stays in one spot.
Floaters are normal in an elderly person b/c as you age, the vitreous naturally weakens. But in a 26 year old, that part of your eye is very firm. The vitreous fluid is like jelly and when it pulls away from the back of the eye, it can cause retinal tears. These tears can then lead to retinal detachment. So in essense, these injections are turning my eyes into that of a 75 year old and as far as I'm concerned, doing a much harm as good.
I'm working with my PCP & RS on getting to a doctor at the Cleveland Clinic.. We have to submit several letters of recommendation to my insurance company in order to convince them to cover the treatments out-of-network. I'm also hoping that Dr. Gindzen can convince the insurance company to cover Lucentis injections since that's the FDA drug instead of Avastin, which is what I'm currently using. Hopefully the smaller molecules will do less damage and will lessen the floaters.
Due to the floaters and vision loss from my first bleed, I'm starting to have alot of trouble driving, esp at night or when my eyes are tired. I've been invited to a luncheon by the Disability Advocates this month, so hopefully I can start getting involved with that group and advocate for better public transportation in our area of town. Its a great group in Grand Rapids, and they do alot of good work for the disable.
So, that's about it. I would love some feedback from others struggling with POHS, especially if you are dealing with floaters that won't go away. Otherwise, thank you for all your prayers and please don't stop praying for my struggle with this disease as well as others who deal with this every day.
God Bless!
Rebecca
Tuesday, April 8, 2008
2nd Treatment Down
Well, last Thursday I had my second treatment of Avastin. After the first, I told myself that with every treatment, it would get easier. Man, was I wrong. This treatment hurt worse than the first and my reaction was worse.
When I had my first intravitreal injection of Avastin, I drove home afterwards; not sure how, but I did. I also went to work the next day. It hurt to work on a computer and be in the light, but I did it nonetheless. After my treatment last Thursday, I could not open my eye at all. I'm so thankful Steve took me to my appointment b/c I would have been sleeping at the doctor's office as there was no way I could have gotten home without him. The next morning, my eye was nearly swollen shut and remained that way all day. My vision was also blurred, so going to work wasn't an option.
The good news is, so far, the treatments are working, and there is a chance that I won't have to have a 3rd treatment on May 1st. I'd be so happy if I only needed an injection every 6-8 weeks instead of every 4 ... of course, to never have to have one again would be the best!
What really gets me is that down the hall, 3 elderly people were getting the same injections. I can't imagine being 80 years old and having needles stuck in my eye. They shouldn't have to go through that.
I really pray that a new treatment is found soon. Avastin is a great temporary drug, but we need something long-term. So, to all the brilliant researchers out there, please, GET TO WORK!
Thursday, March 27, 2008
A breath of fresh air
I went to the doctor this week for a last minute appointment as I noticed a new blurry spot in my right eye. Fortunately, Dr. Gindzen didn't see anything and the OCT scan showed nothing in that area, so we are just going to keep an eye on it for now ... no pun intended! :)
The other bit of good news is that the avastin injection is working. The spot we saw 3 weeks ago is now gone. The OCT did finally show the leakage, and its still there along with the blurriness it caused, but the leaking blood vessel has gone back to its rightful home. I have my 4 week check up on April 3 to see if it is still working.
Praise the Lord for this blessing of good news!
The other bit of good news is that the avastin injection is working. The spot we saw 3 weeks ago is now gone. The OCT did finally show the leakage, and its still there along with the blurriness it caused, but the leaking blood vessel has gone back to its rightful home. I have my 4 week check up on April 3 to see if it is still working.
Praise the Lord for this blessing of good news!
Tuesday, March 11, 2008
My Story
NASHVILLE, TENNESSE
In April of 2005, I was in my last semester of college at Lipscomb University when I lost the vision in my left eye. I had just gotten back from Spring Break in Cancun with my mom, Katie & Patti when the unheard of happened.
I lived alone at the time, and as I was getting ready for school one morning, while putting on my eye liner, I realized that I could no longer see myself when I closed my right eye. This was very upsetting as I'd had vision corrective surgery in February of 2002 ... so for my eyes to be anything other than 20/15, something was obviously wrong.
My grandmother took me to see my eye doctor, and you know something isn't good when your doctor unnervingly gasps. He felt it was either a tumor or Choroidial Neo-Vascularization (CNV). He sent me to a retina specialist who diagnosed me with CNV and said the root of the problem was idiopathic. I then went through 3 laser surguries called photocoagulation with an additional round of steriods. As of April 2007, I was pronounced stable with no office visits for a year, and only a 5% chance of getting the same disease in my right eye.
GRAND RAPIDS, MICHIGAN
On July 21, 2007, Steve and I were married and moved to Grand Rapids, Michigan on August 4th. Having to re-establish myself with new doctors, I quickly made an appointment at Grand Rapids Ophthalmology. It wasn't long before I had an appointment with Dr. Yosef Gindzen, one of the top retina specialists in the country. On my first office visit, he asked me if I grew up near the Mississippi River. It was that day I learned about Ocular Histoplasmosis.
*** Fact ****
In the United States, the highest incidence of histoplasmosis occurs in a region often referred to as the "Histo Belt," where up to 90% of the adult population has been infected by histoplasmosis. This region includes all of Arkansas, Kentucky, Missouri, Tennessee, and West Virginia as well as large portions of Alabama, Illinois, Indiana, Iowa, Kansas, Louisiana, Maryland, Mississippi, Nebraska, Ohio, Oklahoma, Texas, and Virginia. Since most cases of histoplasmosis are undiagnosed, anyone who has ever lived in an area known to have a high rate of histoplasmosis should consider having their eyes examined for histo spots.
**********************
Dr. Gindzen noticed histospots (CNV) in my right eye located right at my central vision. Though they were smaller and fewer in number than those in my left eye, they were there nonetheless, sending that 5% chance of activity to nearly 100% ... vision loss inevitable and dependent only on when the little terriorists woke up and decided to grow. Now, my left eye, which was pronounced "stable" less than a year ago, already had new growth activity and blood leakage, but we've decided not to treat it at the moment since there is already no central vision. Once it begins to expand into what peripheral vision I have left, we'll begin Avastin injections.
Every morning I look at my Amsler Grid to note any changes in vision. Three weeks ago, my right eye grid became distorted. A growth had woken up and was making itself known. Yesterday, March 10, 2008, I began Avastin injections for the first time in my right eye. Waiting those three weeks has thrown my overall vision off enough to cause daily headaches and night driving to be even more difficult, but I have faith I'll adjust to that change soon. There is a 40% chance that the Avastin injections will work and the distortion in my only good eye will be restored to normal.
Unlike photocoagulation treatments which left me with scarred tissue causing permanent blindness at my macula (central vision), Avastin injections leave no scarring, except that one could need them as often as every 4-6 weeks ... sometimes indefinitely. I've spoken to some people who've been getting these intravitreal injections for years. I can't even imagine going through that but I've started the journey now, so pretty soon, I will be one of them ... A Histo Groupie.
I have added some information below about Ocular Histoplasmosis Syndrome. This is not a widely known disease and most people who are carriers have no idea the kind of monster that lies in their system. Thankfully, most people's immune systems are strong enough to kick this nasty disease ... only experiencing symptoms of a common cold or flu. But those who are physically and emotionally impacted by OHS struggle with it for a lifetime as it never fully goes away.
Thank you for reading my story and I hope, in some way, I was able to provide some information about OHS through my personal experience and the collection of data below. On behalf of myself and other OHS victims, please keep us all in your prayers as we struggle daily with our present vision lost as well as knowing that a near end is not in sight.
Subscribe to:
Comments (Atom)
Another victim to POHS
My name is Rebecca. I was officially diagnosed with Ocular Histoplasmosis Syndrome in January of 2008. I grew up in Nashville, Tennessee and had never heard of the fungus Histoplasma Capsulatum until after moving to Grand Rapids, Michigan in August of 2007.
It is my hope from this blog that I can provide information to others about this terrible disease and urge people within the "Histo Belt" to check their sight on a regular basis.
It is my hope from this blog that I can provide information to others about this terrible disease and urge people within the "Histo Belt" to check their sight on a regular basis.
INTERESTING VIDEOS
I've added some interesting videos of different retinal surgeries. I will warn you that these can be graphic, but if you're interested in knowing what surgeries have been done and how they work, take a peek!
Vitrectomy for Vitreous Opacities (Floaters)
Floaters - What are they? How do they happen?
Removal of Subretinal Neovascular Membrane due to OHS
Vitrectomy Surgery
Vitrectomy Surgery allows the Retina Surgeon to work inside of the eye and repair damage caused by a variety of diseases. The vitreous is the jelly inside the eye and is removed during the vitrectomy. YOU DO NOT NEED YOUR VITREOUS. The vitreous is important when the eye forms as a fetus grows into a baby, but it does nothing good for you after that. The vitreous is replaced with a salt solution or gas or oil and your body replaces the salt solution or gas in the vitreous cavity over a week or two.
Some vitrectomies can be performed using very small 25 gauge instruments. Most are done with 20 gauge instrument. Once the vitreous is removed, instruments like picks, forceps, lasers, and cautery can be used inside the eye to help fix problems like macular pucker, macular hole, retinal detachment, vitreous hemorrhage, diabetic retinal disease, infection, retained lens fragments and so on.
Vitrectomy surgery in our practice is usually done with local anesthesia and sedation. Since you will be sedated, YOU CANNOT EAT the morning of surgery. You will be sedated and your eye will be anesthetized. You will be monitored by an anesthesiologist or nurse anesthetist. After surgery you will have to wear a patch and shield over the eye until your appointment the following day.
If you have a retinal detachment and your doctor puts a gas or oil to hold your retina in place, you will have to hold your head in a certain position and also look in a certain position for the surgery to work. This is also true of surgery for macular holes which requires face down positioning.
After your patch is removed during your post-operative visit, you will need to take eye drops. If during the week after surgery, your eye starts to hurt more or vision starts to decline, you should call our office since that can indicate a problem with infection or elevated intraocular pressure. If you see a new shadow after surgery you need to call so we can check to make sure you do not have a retinal detachment.
Using modern microsurgical techniques, your retinal surgeon is able to repair many macular and retinal problems that were once thought unfixable. Your physician can tell you what the success rates are for your surgery including the possibility of some vision improvement and the possibility of a lot of vision improvement.
After any eye surgery there is a risk of infection, bleeding, and retinal detachment. Also, the intraocular pressure in the eye can sometimes rise necessitating extra post-operative eye drops. Make sure to call our office if you are having any problems.
Some vitrectomies can be performed using very small 25 gauge instruments. Most are done with 20 gauge instrument. Once the vitreous is removed, instruments like picks, forceps, lasers, and cautery can be used inside the eye to help fix problems like macular pucker, macular hole, retinal detachment, vitreous hemorrhage, diabetic retinal disease, infection, retained lens fragments and so on.
Vitrectomy surgery in our practice is usually done with local anesthesia and sedation. Since you will be sedated, YOU CANNOT EAT the morning of surgery. You will be sedated and your eye will be anesthetized. You will be monitored by an anesthesiologist or nurse anesthetist. After surgery you will have to wear a patch and shield over the eye until your appointment the following day.
If you have a retinal detachment and your doctor puts a gas or oil to hold your retina in place, you will have to hold your head in a certain position and also look in a certain position for the surgery to work. This is also true of surgery for macular holes which requires face down positioning.
After your patch is removed during your post-operative visit, you will need to take eye drops. If during the week after surgery, your eye starts to hurt more or vision starts to decline, you should call our office since that can indicate a problem with infection or elevated intraocular pressure. If you see a new shadow after surgery you need to call so we can check to make sure you do not have a retinal detachment.
Using modern microsurgical techniques, your retinal surgeon is able to repair many macular and retinal problems that were once thought unfixable. Your physician can tell you what the success rates are for your surgery including the possibility of some vision improvement and the possibility of a lot of vision improvement.
After any eye surgery there is a risk of infection, bleeding, and retinal detachment. Also, the intraocular pressure in the eye can sometimes rise necessitating extra post-operative eye drops. Make sure to call our office if you are having any problems.
What is Histoplasmosis?
Histoplasmosis is a disease caused when airborne spores of the fungus Histoplasma capsulatum are inhaled into the lungs, the primary infection site. This microscopic fungus, which is found throughout the world in river valleys and soil where bird or bat droppings accumulate, is released into the air when soil is disturbed by plowing fields, sweeping chicken coops, or digging holes.
Histoplasmosis is often so mild that it produces no apparent symptoms. Any symptoms that might occur are often similar to those from a common cold. In fact, if you had histoplasmosis symptoms, you might dismiss them as those from a cold or flu, since the body's immune system normally overcomes the infection in a few days without treatment.
However, histoplasmosis, even mild cases, can later cause a serious eye disease called ocular histoplasmosis syndrome (OHS), a leading cause of vision loss in Americans ages 20 to 40.
Histoplasmosis is often so mild that it produces no apparent symptoms. Any symptoms that might occur are often similar to those from a common cold. In fact, if you had histoplasmosis symptoms, you might dismiss them as those from a cold or flu, since the body's immune system normally overcomes the infection in a few days without treatment.
However, histoplasmosis, even mild cases, can later cause a serious eye disease called ocular histoplasmosis syndrome (OHS), a leading cause of vision loss in Americans ages 20 to 40.
Where does Ocular Histoplasmosis Syndrome come from?
Scientists believe that Histoplasma capsulatum (histo) spores spread from the lungs to the eye, lodging in the choroid, a layer of blood vessels that provides blood and nutrients to the retina. The retina is the light-sensitive layer of tissue that lines the back of the eye. Scientists have not yet been able to detect any trace of the histo fungus in the eyes of patients with ocular histoplasmosis syndrome. Nevertheless, there is good reason to suspect the histo organism as the cause of OHS.
What are the symptoms of OHS?
OHS usually has no symptoms in its early stages; the initial OHS infection usually subsides without the need for treatment. This is true for other histo infections; in fact, often the only evidence that the inflammation ever occurred are tiny scars called "histo spots," which remain at the infection sites. Histo spots do not generally affect vision, but for reasons that are still not well understood, they can result in complications years--sometimes even decades--after the original eye infection. Histo spots have been associated with the growth of the abnormal blood vessels underneath the retina.
In later stages, OHS symptoms may appear if the abnormal blood vessels cause changes in vision. For example, straight lines may appear crooked or wavy, or a blind spot may appear in the field of vision. Because these symptoms indicate that OHS has already progressed enough to affect vision, anyone who has been exposed to histoplasmosis and perceives even slight changes in vision should consult an eye care professional.
In later stages, OHS symptoms may appear if the abnormal blood vessels cause changes in vision. For example, straight lines may appear crooked or wavy, or a blind spot may appear in the field of vision. Because these symptoms indicate that OHS has already progressed enough to affect vision, anyone who has been exposed to histoplasmosis and perceives even slight changes in vision should consult an eye care professional.
How is OHS Diagnosed?
An eye care professional will usually diagnose OHS if a careful eye examination reveals two conditions: (1) The presence of histo spots, which indicate previous exposure to the histo fungus spores; and (2) Swelling of the retina, which signals the growth of new, abnormal blood vessels. To confirm the diagnosis, a dilated eye examination must be performed. This means that the pupils are enlarged temporarily with special drops, allowing the eye care professional to better examine the retina.
If fluid, blood, or abnormal blood vessels are present, an eye care professional may want to perform a diagnostic procedure called fluorescein angiography. In this procedure, a dye, injected into the patient's arm, travels to the blood vessels of the retina. The dye allows a better view of the CNV lesion, and photographs can document the location and extent to which it has spread. Particular attention is paid to how close the abnormal blood vessels are to the fovea.
If fluid, blood, or abnormal blood vessels are present, an eye care professional may want to perform a diagnostic procedure called fluorescein angiography. In this procedure, a dye, injected into the patient's arm, travels to the blood vessels of the retina. The dye allows a better view of the CNV lesion, and photographs can document the location and extent to which it has spread. Particular attention is paid to how close the abnormal blood vessels are to the fovea.
Information on systemic histoplasmosis can be obtained from:
The National Institute of Allergy and Infectious Diseases (NIAID)The National Institutes of Health
Building 31, Room 7A50
31 Center Drive, MSC 2520
Bethesda, MD, 20892-2520
Telephone: 301-496-5717
Website: http://www.niaid.nih.gov
Building 31, Room 7A50
31 Center Drive, MSC 2520
Bethesda, MD, 20892-2520
Telephone: 301-496-5717
Website: http://www.niaid.nih.gov