New treatments involving the retina are typically conducted on AMD patients b/c their condition can be proven. OHS is very hard, if not impossible, to prove b/c the fungus is not present ... OHS patients wait for testing to be done on AMD patients, and then we undergo the same procedures and typically get the same results. Unfortunatley, its usually not covered by our insurance as they like to see factual proof of a condition. Regardless, this break through in stem cell research is a very big step forward for both AMD and OHS patients.
The article:
Macular degeneration is a retinal degenerative disease that causes progressive loss of central vision. The risk of developing Macular degeneration increases with age. The disease most often affects people in their sixties and seventies. Macular degeneration is the most common cause of vision loss in individuals over the age of fifty.
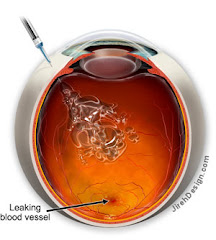
The macula is the central portion of the retina responsible for perceiving fine visual detail. Light sensing cells in the macula, known as photoreceptors, convert light into electrical impulses and then transfer these impulses to the brain via the optic nerve. Central vision loss from Macular degeneration occurs when photoreceptor cells in the macula degenerate.
The Xcell-Center Macular Degeneration treatment
The stem cells are first collected from a patient’s bone marrow, extracted from the hipbone (iliac crest) then implanted back into the body days later. Prior to re-implantation of the cells, the bone marrow is processed in one of our labs, where the quantity and quality of the stem cells is also checked.
These re-injected stem cells have the potential to transform into multiple types of cells and are capable of regenerating damaged tissue. Our innovative stem cell treatments use the self-healing potential of each patient’s own body to stimulate regeneration or repair.
We believe that the retro-bulbar injection of autologous stem cells might first prevent the progression of dry and wet macular degeneration by reducing the Drusen deposits in the retinal pigment epithelium beneath the macula. It might also prevent the destruction of the photoreceptors in both the dry and wet type, by reactivating proper micro-vessel activity and reducing the abnormal blood vessel growth beneath.
Results
The following results are for one female patient, 45 years of age.
In the past, she had undergone several photodynamic laser macula treatments and two "lucentis" intra vitreo injections with a disastrous clinical result. Her clinical condition continued to worsen.
When she arrived at the Xcell-center for the first time, she had a central scotoma on the left eye and she was not able to count her fingers. In the right eye we observed the onset of macula degeneration with macula epiteliopathy and 9/10 corrected visual acuity that we have been able to preserve until the present.
After some detoxification treatments the patient was sent to the XCell-center on April 25, 2008 for a bilateral autologous stem cell retro-bulbar implantation.
Just two weeks after the treatment, during an objective, standardized examination, this patient showed significant improvement.
The next picture shows the Threshold Fovea Map. Clearly visible is the improvement in retinal sensitivity.

The following picture shows the Visual Fields. Here, too, one can see an improved retinal sensitivity.

Macular degeneration is a retinal degenerative disease that causes progressive loss of central vision. The risk of developing Macular degeneration increases with age. The disease most often affects people in their sixties and seventies. Macular degeneration is the most common cause of vision loss in individuals over the age of fifty.
The macula is the central portion of the retina responsible for perceiving fine visual detail. Light sensing cells in the macula, known as photoreceptors, convert light into electrical impulses and then transfer these impulses to the brain via the optic nerve. Central vision loss from Macular degeneration occurs when photoreceptor cells in the macula degenerate.
The Xcell-Center Macular Degeneration treatment
The stem cells are first collected from a patient’s bone marrow, extracted from the hipbone (iliac crest) then implanted back into the body days later. Prior to re-implantation of the cells, the bone marrow is processed in one of our labs, where the quantity and quality of the stem cells is also checked.
These re-injected stem cells have the potential to transform into multiple types of cells and are capable of regenerating damaged tissue. Our innovative stem cell treatments use the self-healing potential of each patient’s own body to stimulate regeneration or repair.
We believe that the retro-bulbar injection of autologous stem cells might first prevent the progression of dry and wet macular degeneration by reducing the Drusen deposits in the retinal pigment epithelium beneath the macula. It might also prevent the destruction of the photoreceptors in both the dry and wet type, by reactivating proper micro-vessel activity and reducing the abnormal blood vessel growth beneath.
Results
The following results are for one female patient, 45 years of age.
In the past, she had undergone several photodynamic laser macula treatments and two "lucentis" intra vitreo injections with a disastrous clinical result. Her clinical condition continued to worsen.
When she arrived at the Xcell-center for the first time, she had a central scotoma on the left eye and she was not able to count her fingers. In the right eye we observed the onset of macula degeneration with macula epiteliopathy and 9/10 corrected visual acuity that we have been able to preserve until the present.
After some detoxification treatments the patient was sent to the XCell-center on April 25, 2008 for a bilateral autologous stem cell retro-bulbar implantation.
Just two weeks after the treatment, during an objective, standardized examination, this patient showed significant improvement.
The next picture shows the Threshold Fovea Map. Clearly visible is the improvement in retinal sensitivity.

The following picture shows the Visual Fields. Here, too, one can see an improved retinal sensitivity.